The key difference between Interstitial Lung Disease and Bronchiectasis is that the interstitial lung diseases are a set of restrictive lung diseases whereas the bronchiectasis is an obstructive lung disease.
Interstitial lung diseases (ILD) are a heterogeneous group of disorders that involve the lung parenchyma – alveolar lining, alveolar walls, capillary endothelium and connective tissue. The same pathological changes caused by infectious agents are not considered as interstitial lung diseases. Bronchiectasis is a pathological condition of the respiratory system characterized by the presence of abnormally and permanently dilated airways.
CONTENTS
1. Overview and Key Difference
2. What is Interstitial Lung Disease
3. What is Bronchiectasis
4. Similarities Between Interstitial Lung Disease and Bronchiectasis
5. Side by Side Comparison – Interstitial Lung Disease vs Bronchiectasis in Tabular Form
6. Summary
What is Interstitial Lung Disease?
Interstitial lung diseases (ILD) are a heterogeneous group of disorders that involve the lung parenchyma – alveolar lining, alveolar walls, capillary endothelium and connective tissue. Same pathological changes caused by infectious agents are not considered as interstitial lung diseases. In almost all the patients there is a fibrosis of the lung parenchyma sometimes with associated inflammation. Ultimately the alveolar septae get thickened impairing the diffusion of oxygen across them.
In the most advanced stage of the disease, there is diffuse fibrosis of the lung giving rise to the characteristic honeycomb appearance in the CT radiographs. The patient may have significant impairment of pulmonary function, pulmonary hypertension, and cor pulmonale.
Common Clinical Features
Common clinical features of interstitial lung disease include;
- Progressive dyspnoea and tachypnoea
- End respiratory crackles (usually no wheezing or other evidence of airway obstruction)
- cyanosis
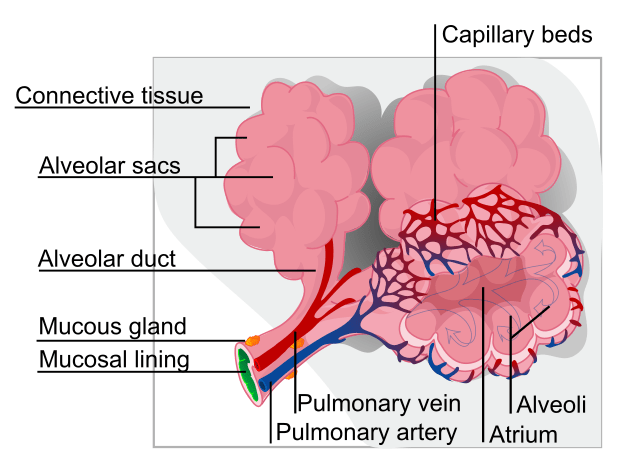
Figure 01: An alveolus in the Lung
Lung Function Tests
- Reduced total lung capacity due to reduced compliance – restrictive type of lung disease
- Reduced CO diffusing capacity
- Chest X-ray
Diffuse infiltrative pattern – small nodules, irregular lines or ground glass shadow
Cause
The exact cause of, a majority of the interstitial lung diseases has not yet been identified. But they are believed to have associations with the following risk factors.
- Exposure to environmental hazards ( commonly smoking, others: industrial exposures)
- Sarcoidosis
- Collagen vascular diseases
- Granulomatous vasculitis (e.g, Wegener’s, Churg – Strauss)
- Hypersensitivity pneumonitis (organic dust)
- Exposure to inorganic dust – beryllium, silica ( predominantly in industrial exposures)
Histological Subtypes of Interstitial Lung Diseases
Investigations
Interstitial lung disease can be investigated via;
- Chest Xray – bilateral reticular pattern. In granulomatous types could be nodular opacities
- HRCT – better assessment of extent and distribution of disease
- Pulmonary function testing – extent of pulmonary involvement is assessed
- Diffusing capacity – reduced the diffusing capacity of the lung for CO
- Arterial blood gas
- Bronchoscopy and bronchoalveolar lavage
- Lung biopsy
- Others:
- In CTDs – ANA, anti-dsDNA, rheumatoid factor
- LDH – a nonspecific finding in ILDs
Management
The management plan can vary depending on the underlying cause of the interstitial lung disease
- Corticosteroids are given to arrest the ongoing inflammatory processes
- The use of immunosuppressants is also advocated in some cases when there is no improvement in the patient’s condition with the corticosteroids alone.
- However, in the most advanced cases, lung transplant remains the only option
What is Bronchiectasis?
Bronchiectasis is a pathological condition of the respiratory system characterized by the presence of abnormally and permanently dilated airways. As a result of the chronic inflammation, bronchial walls get thickened and irreversibly damaged. The impairment of the mucociliary transport mechanism increases the risk of superimposed infections.
Etiology
The causes of bronchiectasis are;
- Congenital defects such as deficiency of bronchial wall elements and pulmonary sequestration
- Obstruction of the bronchial wall due to mechanical causes such as tumors
- Postinfective bronchial damage
- Granuloma formation in conditions such as tuberculosis and sarcoidosis
- Diffuse diseases of the lung parenchyma such as pulmonary fibrosis
- Immunological overresponse in conditions such as post lung transplant
- Immune deficiencies
- Mucociliary clearance defects in diseases such as cystic fibrosis
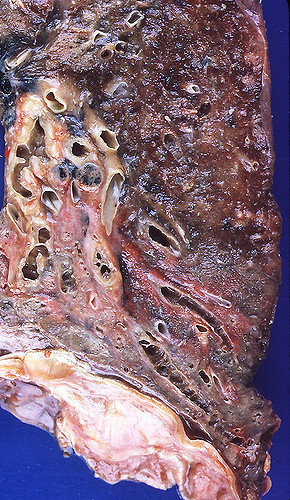
Figure 02: Bronchiectasis
Clinical Features
The clinical features of bronchiectasis include;
- The production of green or yellow color sputum is the only clinical manifestation in mild bronchiectasis
- With the disease progression, the patient can get other serious symptoms such as persistent halitosis, recurrent febrile episodes with malaise and recurrent bouts of pneumonia.
- Clubbing of the fingernails
- During the auscultation, coarse crackles can be heard over the infected regions
- Breathlessness
- Hemoptysis
Investigations
Investigations of bronchiectasis include;
- Chest X-ray – this usually shows the presence of dilated bronchi with thickened walls. Occasionally multiple cysts filled with fluids can also be observed.
- High-resolution CT scanning
- Examination and culture of sputum are essential for the identification of the etiological agent as well as for the determination of the suitable antibiotics that have to be prescribed in the management of the superimposed infections.
- Sinus X –rays – a majority of the patients can have rhinosinusitis also
- Serum immunoglobulins – this test is performed to identify any immunodeficiencies
- Sweat electrolytes are measured if cystic fibrosis is suspected
Treatment
The treatment and management of bronchiectasis are;
- Postural drainage
- Antibiotics – the type of antibiotic used depends on the causative agent
- It is necessary to use bronchodilators sometimes to avoid the limitations to the airflow
- Anti-inflammatory drugs such as oral or nasal corticosteroids can arrest the disease progression
Complications
- Pneumonia
- Pneumothorax
- Empyema
- Metastatic cerebral abscesses
What is the Similarity Between Interstitial Lung Disease and Bronchiectasis?
- Both conditions are lung diseases
What is the Difference Between Interstitial Lung Disease and Bronchiectasis?
Interstitial lung diseases (ILD) are a heterogeneous group of disorders that involve the lung parenchyma – alveolar lining, alveolar walls, capillary endothelium and connective tissue while Bronchiectasis is a pathological condition of the respiratory system characterized by the presence of abnormally and permanently dilated airways. This is the key difference between Interstitial interstitial lung disease and bronchiectasis. Also, there are othere differences between interstitial lung disease and bronchiectasis based on the cause, clinical features, investigation technique, treatment and management, which are tabulated below.
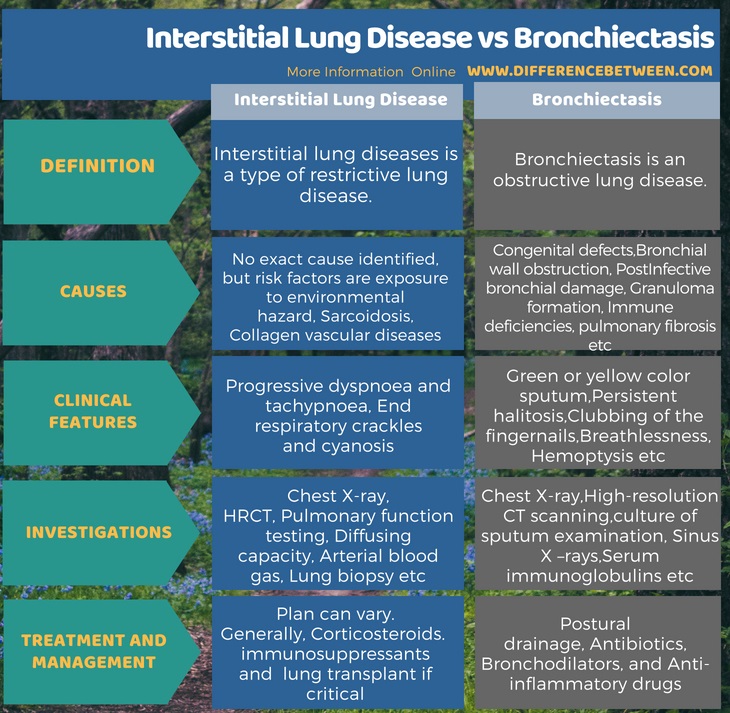
Summary – Interstitial Lung Disease vs Bronchiectasis
Interstitial lung diseases (ILD) are a heterogeneous group of disorders that involve the lung parenchyma – alveolar lining, alveolar walls, capillary endothelium and connective tissue whereas bronchiectasis is a pathological condition of the respiratory system characterized by the presence of abnormally and permanently dilated airways. Bronchiectasis is an obstructive lung disease but interstitial lung diseases are restrictive in nature. This is the major difference between Interstitial Lung Disease and Bronchiectasis.
Reference:
1. Parveen Kumar. Kumar and Clark’s Clinical Medicine. Edited by Michael L Clark, 8th ed.
Image Courtesy:
1.’Alveolus diagram’By LadyofHats – own work (Public Domain) via Commons Wikimedia
2.’3677946871′ by Yale Rosen (CC BY-SA 2.0) via Flickr
ncG1vNJzZmivp6x7pbXFn5yrnZ6YsqOx07CcnqZemLyue8OinZ%2Bdopq7pLGMm5ytr5Wau261za2cq6uknsGqrctmo66ml2Kxqr%2FEmqqeZZGjsW6u0ailnKCZmrC1rdKiqmg%3D