Key Difference – Diverticulitis vs Ulcerative Colitis
In the medical jargon, the suffix “itis” is almost always used to describe something to do with inflammation. According to that preamble, you can understand that diverticulitis is the inflammation of the diverticula that arise from the colon. Ulcerative colitis, on the other hand, is the inflammation of the colon with the formation of associated ulcers. In ulcerative colitis, the overlying mucosa of the colon is inflamed, but in diverticulitis, it is the diverticulum arising from the colon that gets inflamed. This is the key difference between diverticulitis and ulcerative colitis.
CONTENTS
1. Overview and Key Difference
2. What is Diverticulitis
3. What is Ulcerative Colitis
4. Similarities Between Diverticulitis and Ulcerative Colitis
5. Side by Side Comparison – Diverticulitis vs Ulcerative Colitis in Tabular Form
6. Summary
What is Diverticulitis?
Diverticulitis is the inflammation of the diverticula in the colon. These diverticula can be of either congenital or acquired origin.
An inflamed diverticulum can give rise to the following complications.
- The diverticulum can perforate into the peritoneum, resulting in peritonitis. Pericolic abscesses can be formed if it penetrates the pericolic tissues. Its perforation into any other adjacent structure is most likely to end up with the occurrence of fistula.
- The chronic inflammation associated with diverticulitis leads to fibrosis of the inflamed tissues giving rise to obstructive symptoms such as constipation.
- The erosion into blood vessels results in internal hemorrhages.
Clinical Features
Acute Diverticulitis
This condition is known as the left-sided appendicitis because of the characteristic pain of acute onset that originates in the low central region of the abdomen and gradually shifts to the left iliac fossa. There can be other nonspecific symptoms such as nausea, vomiting, local tenderness and guarding.
Chronic Diverticular Disease
This mimics the clinical features of a colonic carcinoma.
- Change in bowel habits
- Vomiting, abdominal bloating, colicky abdominal pain, and constipation due to the obstruction of the large bowel.
- Blood and mucus per rectum

Figure 01: Diverticula of the Sigmoid Colon
Investigations
- CT is the most appropriate investigation to identify diverticulitis in its acute stage by excluding other possible diagnoses.
- Sigmoidoscopy
- Colonoscopy
- Barium enema
Treatment
Acute Diverticulitis
Conservative management is recommended for treating a patient diagnosed with acute diverticulitis. The patient is kept on a fluid diet and antibiotics such as metronidazole and ciprofloxacin.
- Pericolic abscesses are diagnosed by CT. Percutaneous drainage of these abscesses is essential to avoid any future complications.
- In case of a ruptured abscess giving rise to peritonitis, the pus should be removed from the peritoneal cavity by laparoscopic lavage and drainage.
- When there is a diverticulitis associated obstruction in the colon, laparotomy is required to establish the diagnosis.
Chronic Diverticular Disease
This condition is managed conservatively if the symptoms are mild and the diagnosis has been confirmed through investigations. Usually, a lubricant laxative and high fiber containing diet are prescribed. When the symptoms are severe, and the possibility of a colonic carcinoma cannot be excluded laparotomy and resection of the sigmoid colon are carried out.
What is Ulcerative Colitis?
Ulcerative colitis is an inflammatory disease of the rectum, extending proximally to a variable distance. Women are more likely to be affected by this condition than men.
Morphology
The lesions occur in a continuous, uninterrupted manner
Macroscopy varies according to the stage of disease progression. In the acute form of the disease, large bowel is involved in a diffuse continuous manner, and the mucosa has a smooth, velvety appearance. The mucosal layer is easily scraped off. In the chronic stage, there can be ulcers of various sizes. Because of the ulceration of the entire thickness of the mucosa, the adjacent areas appear to be elevated, giving rise to a characteristic morphological feature called pseudopolyps. In the most advanced stage, the entire bowel is shortened, fibrosed and narrowed.
The increased number of inflammatory cells can be observed by the microscopic examination of a biopsy sample taken from the inflamed bowel mucosa. There can be malignant and dysplastic changes also.
Clinical Features
- Blood and mucus diarrhea
- Cramp-like abdominal pain
- Per rectal bleeding
- In some cases, there can be toxemia, fever and severe bleeding.
Investigations
- Sigmoidoscopy
- Colonoscopy
- Barium enema
- Examination of the stools reveals the presence of blood and pus
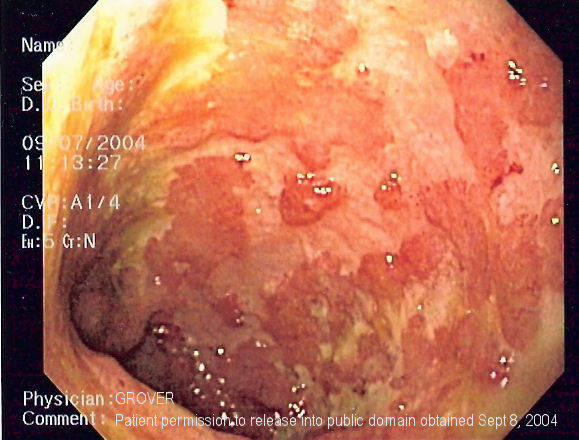
Figure 02: Endoscopic Image of Ulcerative Colitis
Complications
Local Complications
- Toxic dilatation
- Hemorrhage
- Stricture
- Malignant changes
- Perianal diseases such as anal fissures and anal fistulae.
General Complications
- Toxemia
- Anemia
- Weight loss
- Arthritis and uveitis
- Dermatological manifestations such as pyoderma gangrenosum
- Primary sclerosing cholangitis
Management
Medical Management
A high protein diet with vitamin supplements and iron is prescribed. Blood transfusion may be required if the patient shows clinical signs of severe anemia. Loperamide is usually given to control diarrhea. The administration of corticosteroids as per rectal infusions induces remission in an acute attack. Immunosuppressors such as infliximab are required to control more severe attacks of ulcerative colitis.
Surgical Management
Surgical intervention is indicated only in the following situations:
- Fulminating disease not responding to medical treatments
- Chronic disease not responding to medical treatments
- Prophylaxis against malignant changes
- In the occasions where the patient presents with the complications mentioned above.
What is the Similarity Between Diverticulitis and Ulcerative Colitis?
- Both conditions are associated with the inflammation of the affected site.
What is the Difference Between Diverticulitis and Ulcerative Colitis?
Diverticulitis vs Ulcerative Colitis | |
| Diverticulitis is the inflammation of the diverticula in the colon. | Ulcerative colitis is an inflammatory disease of the rectum extending proximally to variable distance. |
| Location | |
| This occurs in the diverticula. | This occurs in the colon. |
| Pathogenesis | |
| There is not enough evidence to suggest a genetic predisposition. Any weakness of the colon, particularly in the distal regions, can contribute to the formation of diverticula. | Genetic predisposition and different environmental factors such as medications and exposure to various pollutants are believed to be the causes of ulcerative colitis. |
| Clinical Features | |
| Change in bowel habits, vomiting, abdominal bloating, colicky abdominal pain (usually in the lower parts of the abdomen), and constipation due to the obstruction of the large bowel are the main clinical features. In rare cases, there can per rectal bleeding when an inflamed diverticulum has ruptured. | Clinical features include blood and mucus diarrhea, rectal bleeding and cramp-like abdominal pain. In addition to that, there can be nonspecific symptoms such as fever, weight loss and aphthous ulcers in the mouth. The continuous loss of blood and decreased absorption of iron can cause anemia. |
| Complications | |
| Hemorrhages and anemia are the main complications. The chance of malignant changes is extremely low. | Toxic megacolon and malignant changes are the most serious complications. In addition, there can be hemorrhages, anemia and associated arthritis. |
| Investigations | |
| CT is the most appropriate investigation to identify diverticulitis in its acute stage by excluding other possible diagnoses. Sigmoidoscopy, colonoscopy and barium enema can also be helpful. | Sigmoidoscopy, colonoscopy, barium enema and examination of the stools to show the presence of blood and pus are the main investigations carried out to diagnose ulcerative colitis. |
| Management | |
| A fluid diet and antibiotics such as metronidazole and ciprofloxacin are prescribed in the management of acute diverticulitis. If the patient has got peritonitis due to the rupture of these abscesses laparoscopic lavage and drainage of the pus is required. | A high protein diet with an abundance of fiber is recommended in the management of ulcerative colitis. Blood transfusion is done only when the patient is severely anemic. Loperamide is usually given to control diarrhea. Corticosteroids given as per rectal infusions counter the inflammatory reactions that give rise to the clinical features. Immunosuppressors such as infliximab are required to control more severe attacks of ulcerative colitis. |
Summary – Diverticulitis vs Ulcerative Colitis
Diverticulitis is the inflammation of the diverticula arising from the colon whereas ulcerative colitis is the inflammation of the colon with the formation of associated ulcers. In the ulcerative colitis the colonic mucosa gets inflamed, but in diverticulitis, the diverticula that originate from the colon are the structures that get inflamed. This is the difference between diverticulitis and ulcerative colitis.
Download PDF Version of Diverticulitis vs Ulcerative Colitis
You can download PDF version of this article and use it for offline purposes as per citation note. Please download PDF version here Difference Between Diverticulitis and Ulcerative Colitis
References:
Image courtesy:
ncG1vNJzZmivp6x7pbXFn5yrnZ6YsqOx07CcnqZemLyue8OinZ%2Bdopq7pLGMm5ytr5Wau26wyK%2Bcq6yZmMKttdOiqmaZnpl6t7%2BMrqOcnaKWwarCxGaaqKSZqba0ew%3D%3D